11 min read • Healthcare & Life Sciences, Operations management
Ambulance services – Optimizing operations
Rethinking emergency services for efficiency


Executive Summary
The global ambulance service market is projected to exhibit steep growth, which will be linked primarily to an aging population, favorable payment policies, and an increase in road accidents. Ambulance service providers need to come up with novel methods to address this rise in demand.
In this paper, Arthur D. Little and Access Health propose a framework that enables concerned stakeholders to identify root causes of inefficiency and, consequently, develop operating models supported by innovative approaches and technologies.
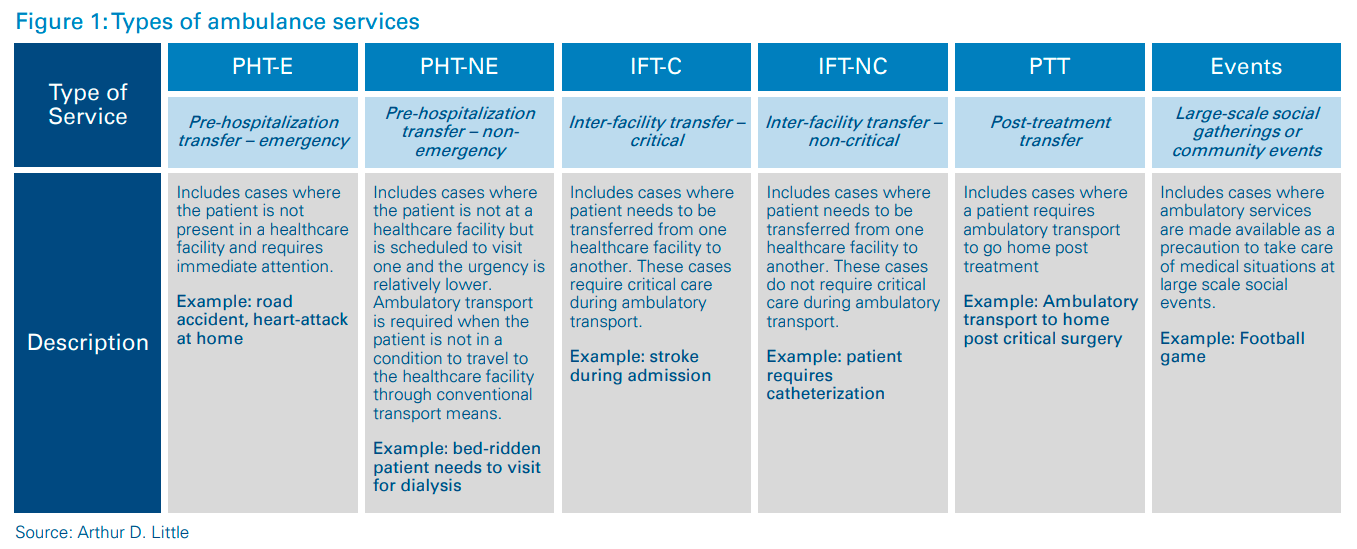
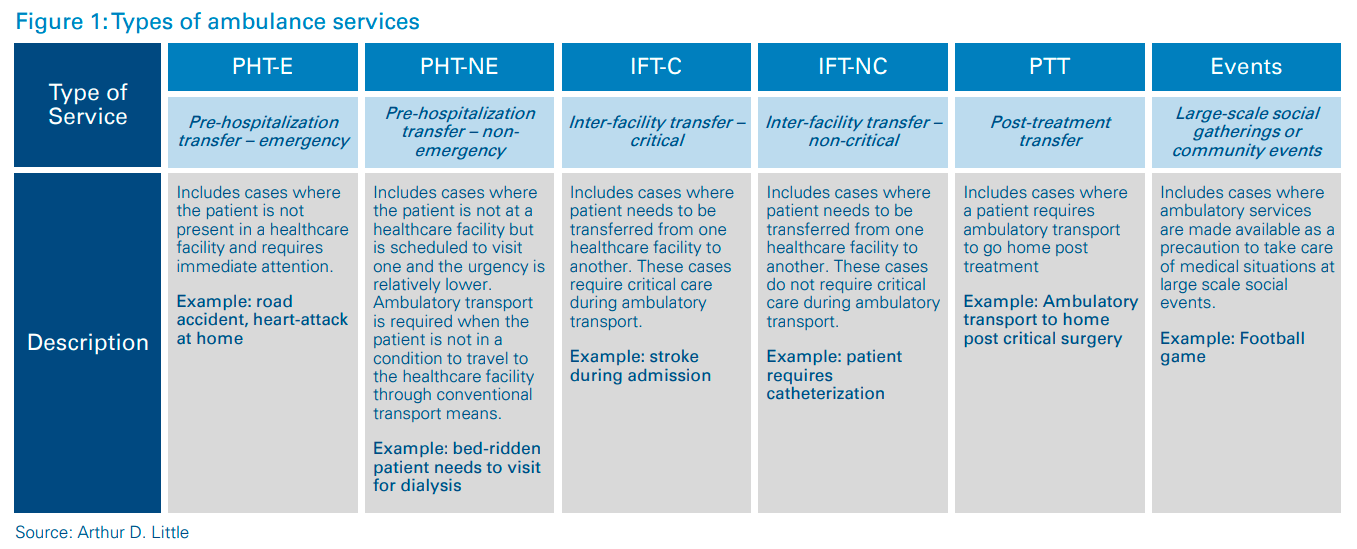
Ambulance services across the globe can be classified into six categories based on criticality, urgency, source and destination, and stage of care. While developing an operating model for ambulance services, it is critical to set the scope of the services because different types should be measured with different sets of KPIs.
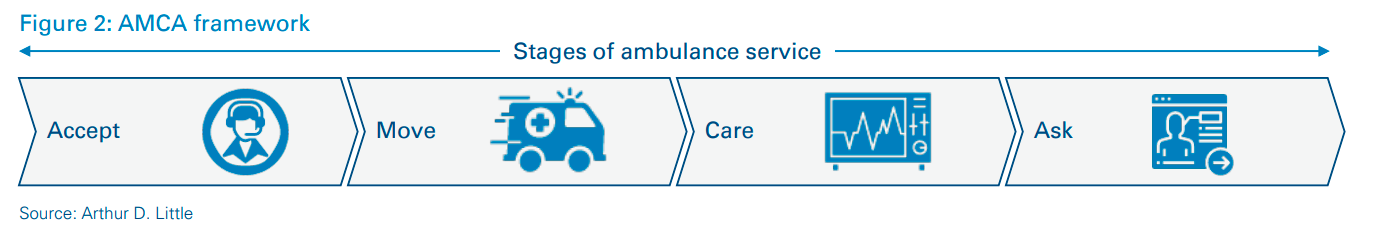
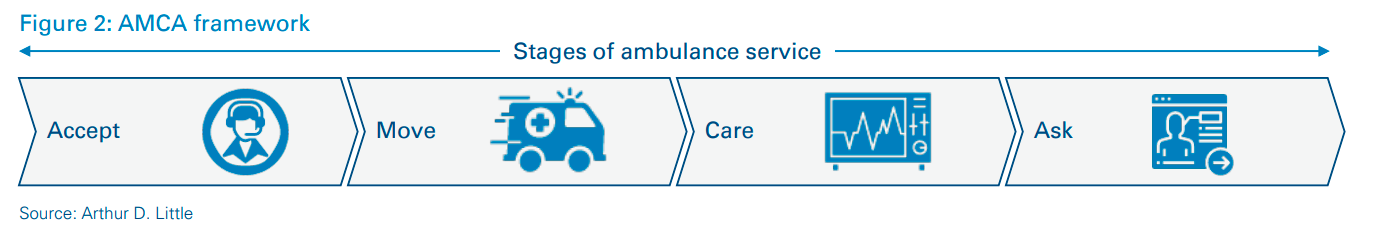
Understanding the value chain and the associated processes in each step is vital to building efficient operating models. Arthur D. Little, in partnership with Access Health, has developed the AMCA1 framework, which helps with critical analysis of the value chain. Deep and thorough understanding of all processes helps to customize the overall operating model to the requirements of different ambulance service categories.
All ambulance services can be mapped into two broad categories of assets: (i) control center and (ii) fleet and equipment; as well as four broad categories of related activities: (i) own, (ii) develop/ maintain, (iii) operate, and (iv) regulate. Arthur D. Little has developed its proprietary “Triple A” (Ambulance Asset and Activity) framework, which enables development of a strategically aligned and efficient operating model.
Building the best operating model for ambulance services based solely on efficiency carries the risk of ignoring factors such as the socio-economic construct, technological maturity of the ecosystem, institutional arrangements between different stakeholders, and involvement of private players.
Lastly, the recipe for a successful operating model is incomplete without innovative solutions. Arthur D. Little recommends developing solutions around the three key levers of ambulance operations: service delivery and asset development, governance and organization, and human capital development.
1
Categorize ambulance services
The global ambulance services market is projected to grow at a CAGR of 9.1 percent and reach approximately USD 50 billion by 20252 . This growth will be driven by three key factors: (i) aging population, (ii) favorable payment policies, and (iii) an increase in road accidents. Extensive growth such as the above can put excessive strain on existing resources, even to maintain the current performance. In order to improve performance levels and meet the increasing demand, ambulance service providers will have to deliver services with higher efficiency and sustainability, as well as improved customer experience.
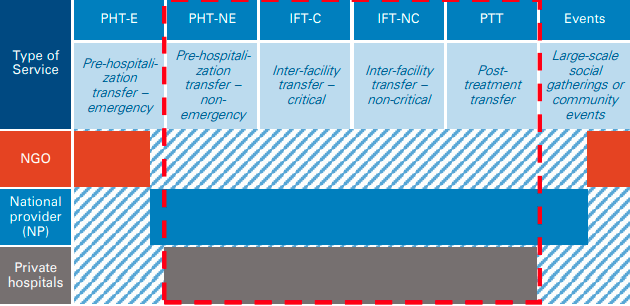
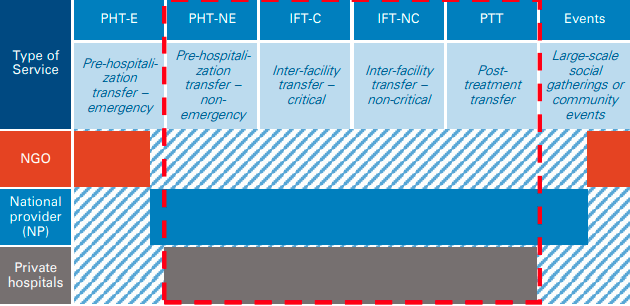
Ambulance services across the globe can be classified into six categories:
- Pre-hospitalization transfer – emergency (PHT-E)
- Pre-hospitalization transfer – non-emergency (PHT-NE)
- Inter-facility transfer – critical (IFT-C)
- Inter-facility transfer – non-critical (IFT-NC)
- Post-treatment transfer (PTT)
- Large-scale gatherings or community events (Events)
These categories are based on:
- Criticality – refers to the patient’s condition and determines
- Urgency – refers to the time limit within which care should ideally be provisioned.
- Source and destination – refers to the location type from which the patient is picked up and handed over.
- Stage of treatment – refers to three different patient-care pathways. These are whether the patient has yet to be hospitalized for treatment, needs to be transported between facilities during the treatment, or must be transported back home post-treatment.
While designing the operating model, it is important to consider which category of service(s) is being planned for. If a provider is responsible for the full spectrum of services, it is imperative that the provider treats different categories as distinct business units with separate resources, while leveraging synergies between them.
Categorization is also useful from a performance management perspective. For example:
- PHT-E and NE should focus on patient outcomes, which might not be of similar significance for PTT and IFT-NC.
- IFT-C and PHT-E should focus on care provided during the ambulance journey, which might not be of similar significance for IFT-NC.
- PHT-E should focus on time to respond, which might not be of similar significance for PHT-NE and PTT.
2
Study the value chain and customize
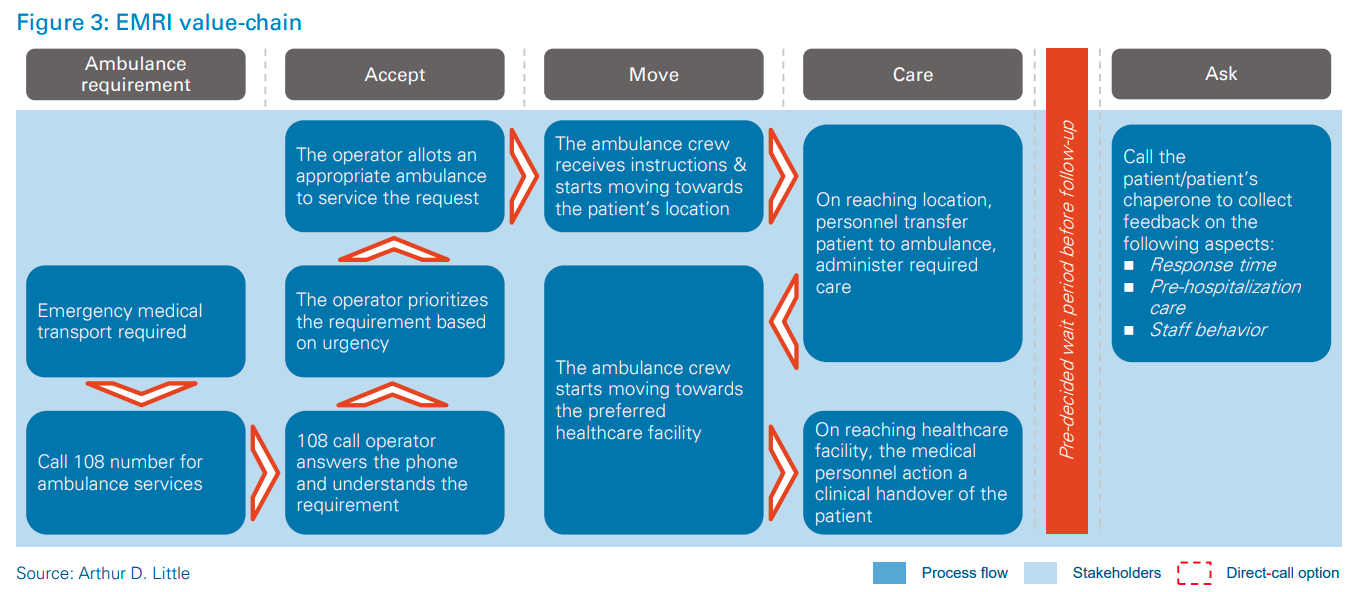
Arthur D. Little has developed its proprietary framework, AMCA (refer to Figure 3), which enables providers to critically analyze the value chain for different types of ambulance services.
Accept – Receiving, accepting and prioritizing requests for ambulance services, and then assigning and dispatching the optimal vehicle and personnel to service each request.
Move – The process of reaching the patient’s location and transporting the patient to the appropriate healthcare facility.
Care – The process of providing care on the way to the healthcare facility, stabilizing the patient, and performing clinical handover at the healthcare facility.
Ask – Collecting feedback on ambulance services and storing the feedback data in a structured and usable format.
Each step along the value chain must be carefully customized for the category requirements. For example:
- Investing in expensive medical equipment for Care in IFT-C and PHT-E will help save lives, but similar investments in IFTNC or PTT would not be able to generate significant value.
- The same feedback questionnaire for Ask in PHT-E and IFT-NC will lead to longer questionnaires to ensure comprehensiveness, which will result in a collection of unnecessary and irrelevant data, as well as missing out on valuable insight.
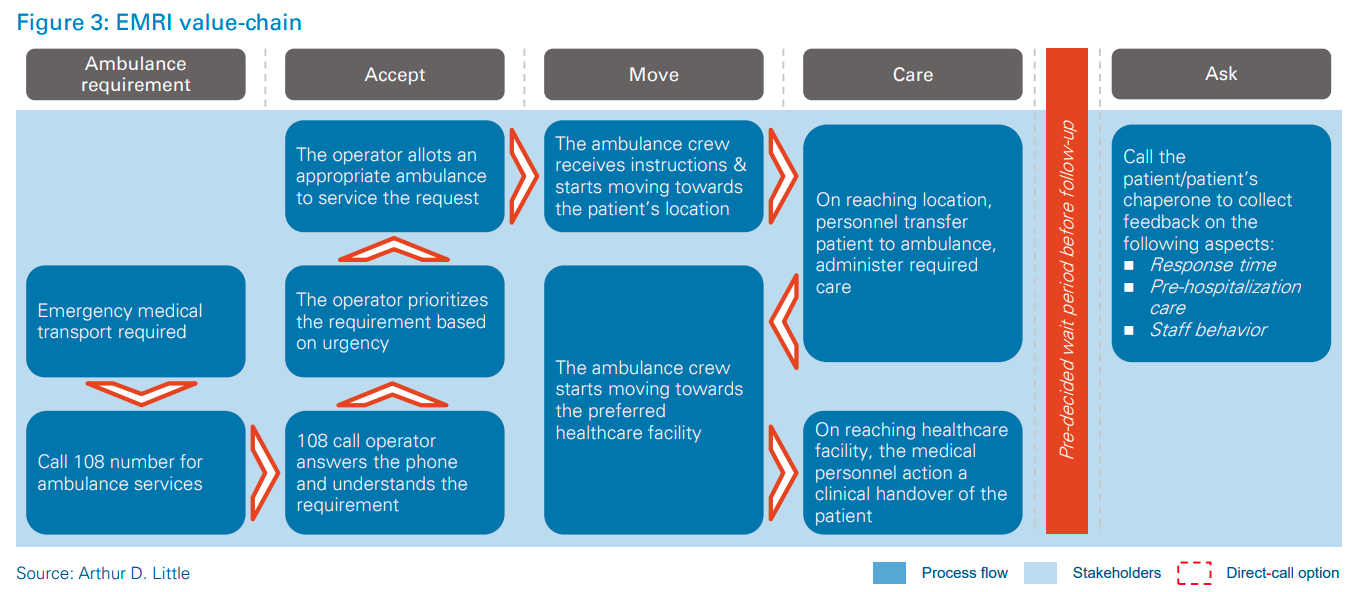
Issues can be identified by deconstructing the ambulance services value chain into AMCA steps, which can be further broken down into specific process steps and KPIs. These issues can then be dealt with to maintain continuous improvement of services. For example, GVK Emergency Management and Research Institute in India has successfully ensured improvement of ambulance services for PHT-E in participating regions by clearly allocating different functions to different steps in the value chain. GVK EMRI’s impact, in the states where it operates, has improved KPIs in line with international benchmarks. For example, GVK EMRI operators can respond to 97 percent of requests on time and dispatch ambulances within an average of 90–120 seconds for emergencies
3
Enable each process with assets and activities
After establishing the process steps required to deliver one or more types of ambulance services, the next step is to identify the stakeholders involved in the ambulance services ecosystem, their respective responsibilities, and the specific contracts and interactions between them.
All types of ambulance services across the globe can be mapped into two broad categories of assets: (i) control center and (ii) fleet and equipment; as well as four wide categories of related activities: (i) own, (ii) develop/maintain, (iii) operate, and (iv) regulate. Arthur D. Little’s proprietary Triple A (Ambulance Asset and Activity) framework enables development of a strategically aligned and efficient operating model. The framework is based on the premise that each process can be mapped to one or more assets and activities for efficient delivery of services
There are four activities associated with each asset type:
Control center
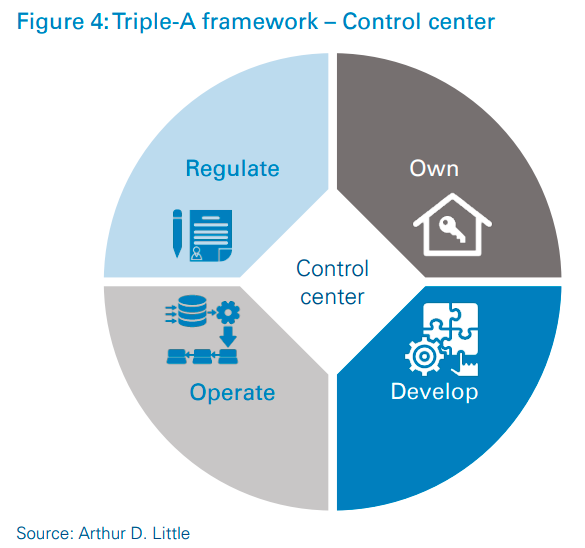
Own – Purchasing the fixed assets (except technology application) required for control center operations.
Develop – Working with a technology vendor to develop the technology solutions for control center operations.
Operate – Executing day-to-day control center operations, including hiring and training of the human resources required for them.
Regulate – Identifying performance KPIs and setting targets to ensure quality and efficiency of service. Ensuring robust performance measurement through audit and supervision.
Fleet and equipment
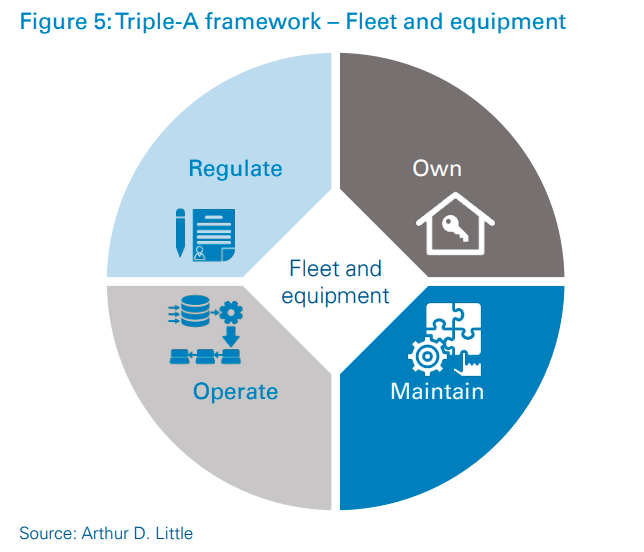
Own – Purchasing the fixed assets (vehicles and medical equipment) required for provision of ambulance move-and-care operations.
Maintain – Maintaining the ambulance fleet and medical equipment used for move-and-care operations.
Operate – Executing day-to-day move-and-care operations, including hiring and training the human resources required for them.
Regulate – Identifying performance KPIs and setting benchmarks to ensure quality and efficiency of service. Ensuring robust performance measurement through inspections.
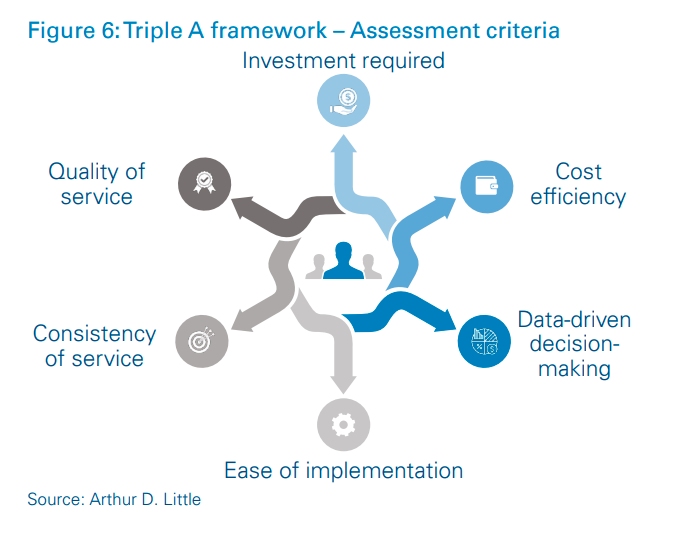
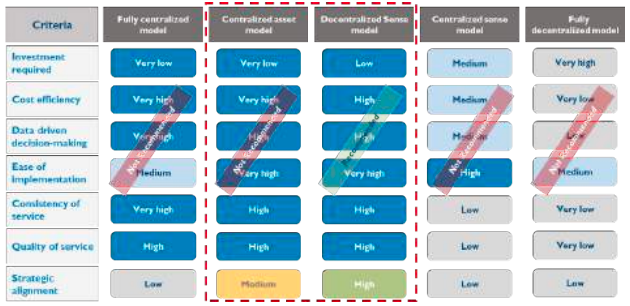
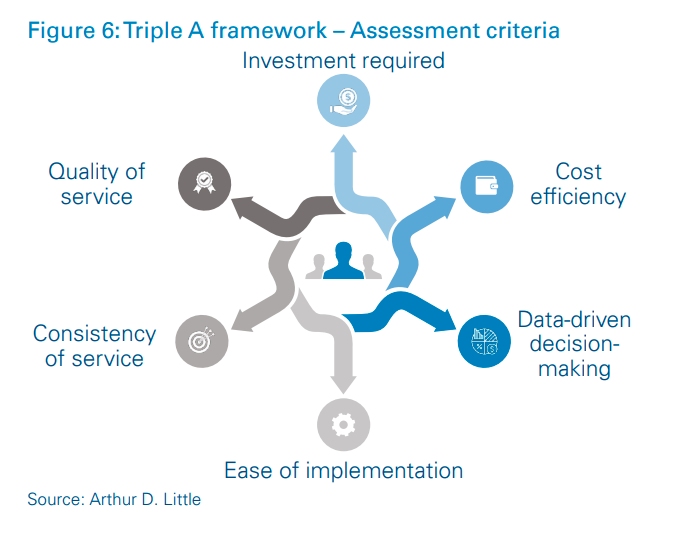
The Triple-A framework can be used to develop strategic options for an operating model based on the divisions of activities within various stakeholder groups. The number and types of stakeholders identified can also vary between strategic options. Arthur D. Little has identified several parameters based on which each strategic option can be evaluated.
Investment required – The parameter for the efficiency of a model in terms of the investment required to set up and run operations.
Cost efficiency – The efficiency of the operations regarding the costs incurred when provisioning services.
Data-driven decision-making – The ease with which data can be collected and analyzed to enable continuous improvement.
Ease of implementation – The effort required for, and the feasibility of, implementing the option’s operating model.
Consistency of service – The degree of service standardization and consistency across regions.
Quality of service – The quality of service (call and care management) that the option’s operating model will be able to deliver
4
Consider the context
Efficiency might not be the most important factor in developing successful operating models. The right operating model must also consider other aspects, such the socio-economic construct, technological maturity, institutional arrangements between stakeholders, and involvement of private players and the community.
For example, a key factor to consider is the institutional arrangement between the national health ministry and the regional health administrations that are responsible for ambulance services. The operating model can be significantly different if the ministry is directly responsible for provision of ambulance services. As demonstrated above, it is important to identify the different institutional arrangements that provide and regulate ambulance services. It is also useful to consider which stakeholder is responsible for financing the operations and which is the payer for the services.
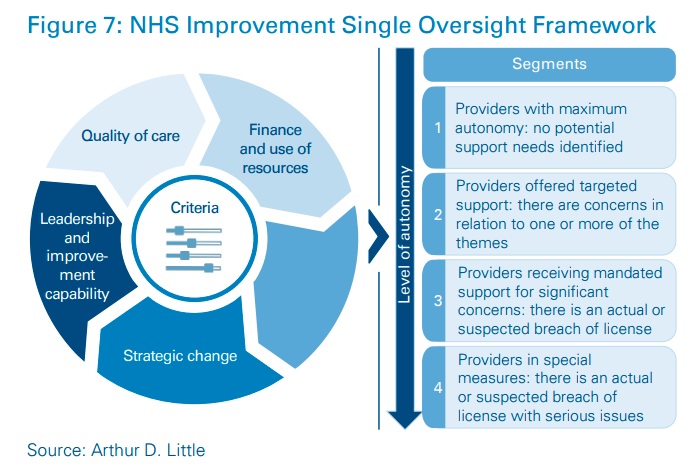
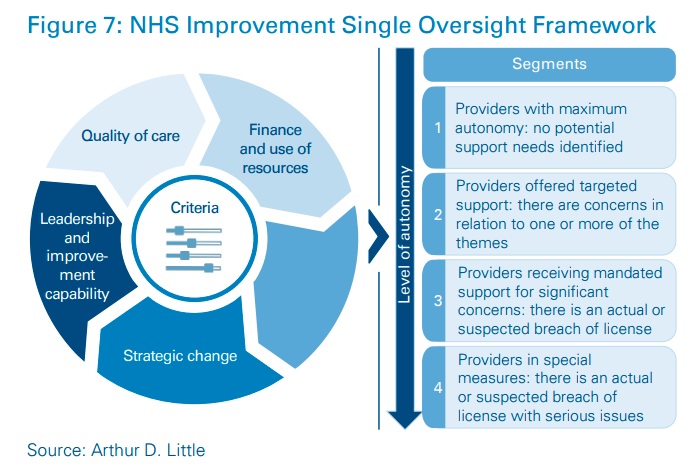
The governance model applied by the National Health Service (NHS) in England, where ambulance services are provisioned through autonomous regional NHS ambulance trusts, ensures effective governance of trusts without direct control. A national body within the NHS, NHS Improvement, benchmarks different trusts against each other, thereby creating a healthy competitive environment in which to learn and improve. As shown in the figure, NHS Improvement uses the Single Oversight Framework to assess trusts’ performance and support needs.
It is also imperative to set the context regarding the intended scale of services. For example, one needs to consider whether the model is being optimized for an ambulance operator with 20 ambulances, a hospital group with 100 ambulances, or a health ministry that provides ambulance services throughout a region or entire country.
Strategic alignment with the “big picture” of the healthcare system is a great example of how focusing solely on operational efficiency can risk long-term aspirations. For example, a healthcare system, which is centralized and wherein the onus of provisioning all types of services lies with the national health ministry, is trying to move towards a system of accountable care organizations (ACOs) based on regions. Assuming that a centralized ambulance service operating model is the most efficient, it will still be in the best interest of the country to choose a sub-optimal model in which a higher share of the responsibility lies with regional health administrations. Otherwise, the country risks hampering its progress towards an ACO model.
As exploring synergies is an immensely useful tool for optimization, it becomes important to identify providers and services with whom ambulance operators can work. For example, GVK Emergency Management and Research Institute in India, which drastically improved ambulance services in India, came up with a system of integrating operations with the police and fire departments to address life-threatening delays to emergency response services. According to GVK EMRI estimates, 18 percent of all emergency calls in India require police intervention. Hence, GVK EMRI ensured that three to six police personnel were stationed at emergency response centers. The move eliminated the need to wait for an emergency call to the police response number, as the personnel could be alerted based on a call to the ambulance number. GVK EMRI also integrated its technology with that of the police to enable the two departments to share valuable information in a seamless and efficient manner.
5
Success is driven by innovation
For an operating model to be optimal, development needs to be supported with innovation. Once each asset and activity is identified, relationships between them can be improved by innovating in the following areas:
- Service delivery and asset development
- Governance and organization
- Human-capital development
Based on an extensive benchmarking study of the most developed ambulance services across the globe, Arthur D. Little identified the following best practices across various areas to create a high-value-generating ambulance ecosystem:
Service delivery and asset development
Leverage technology
- Outsource technology to a technology vendor.
- Enable optimal geo-spatial positioning through technology.
- Use data analytics to identify issues and continuously improve.
Centralize operations
- Centralize services across relevant processes in the value chain for sizable cost reductions.
Improve asset quality
- Secure maintenance contracts with service providers/OEMs to ensure higher quality of fleet and medical equipment.
Governance and organization
Enforce guidelines
- Set comprehensive guidelines and regulations and ensure strict adherence.
- Ensure adherence to well-defined protocols at all levels for smooth and efficient service.
Measure and benchmark performance
- Conduct robust performance measurement, set targets, and link incentives to performance.
- Benchmark providers against each other to help them identify issues.
Structure organization by function
- Organize internal teams by different functions (such as human resources, finance, operations and technology) to achieve a lean and efficient organization structure.
Human capital development
Focus on career development
- Provide a clear career path for paramedical staff to assure them of long-term, sustainable careers and reduce turnover.
- Offer rotation of paramedical staff across units (regions, departments, etc.) to expose the workforce to valuable learning.
Improve access to formal education
- Ensure training of a sufficient number of paramedics by setting up educational institutes from scratch or leveraging existing institutes.>
Mandate continuing professional development
- Define minimum professional standards, conduct audits, and enable the system to upskill its talent
Arthur D. Little’s approach was designed to develop innovative and practical solutions based on careful assessment of the requirements, issues, and capabilities of the ambulance services in question. The assessment is followed by a rigorous benchmarking exercise that enables identification of best practices. We then help our clients develop operating models that take the context into consideration. As a last step, we provide tangible recommendations across the three key areas:
- Service delivery and asset development
- Governance and organization
- Human-capital development
We can support our clients from design to implementation of their ambulance services, depending on their internal requirements.
Case study
1. Categorizing services
The client organization was a GCC health ministry that acted as the regulator and national provider (focused on inter-facility ambulance services-referral transport).
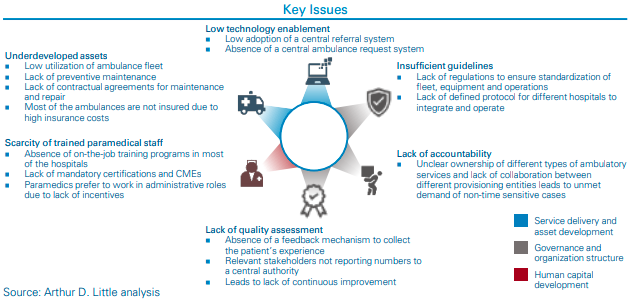
2.Identifying key issues along the value chain
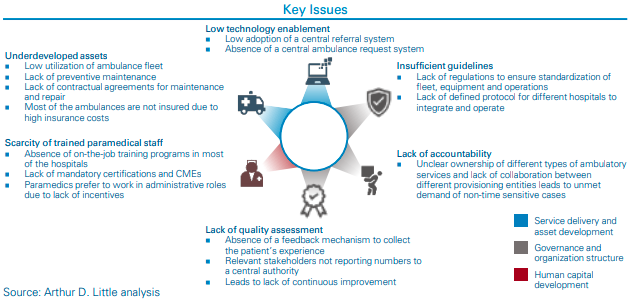
Arthur D. Little segmented the value chain as per the AMCA framework and identified key issues. The health ministry’s decentralized system suffered from problems such as low utilization of assets, shortage of trained paramedics, and low technology adoption.
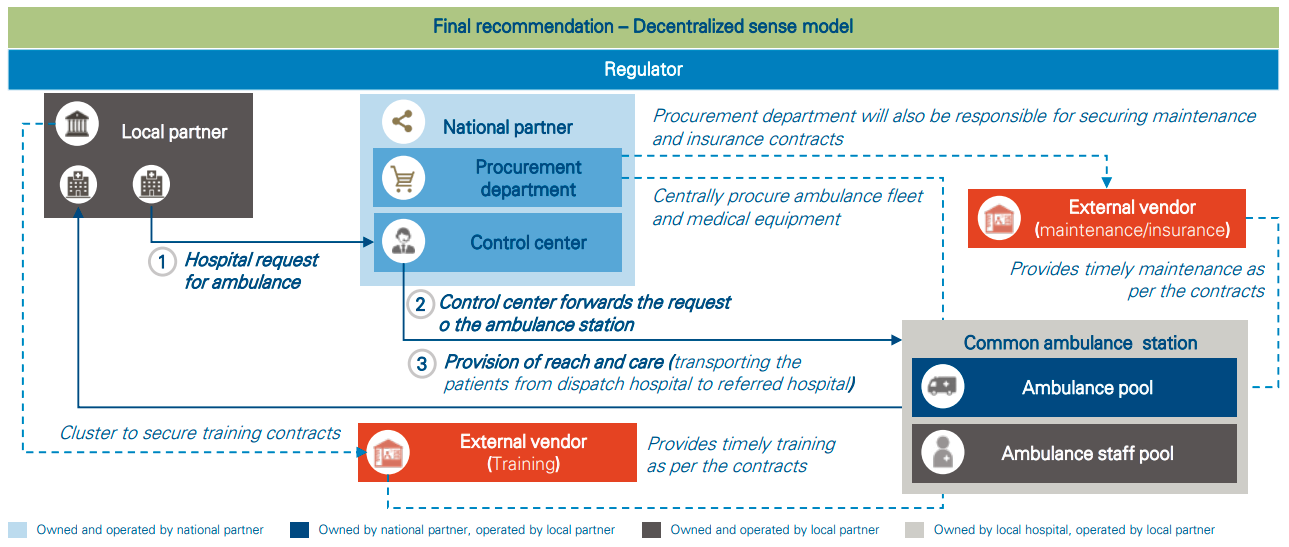
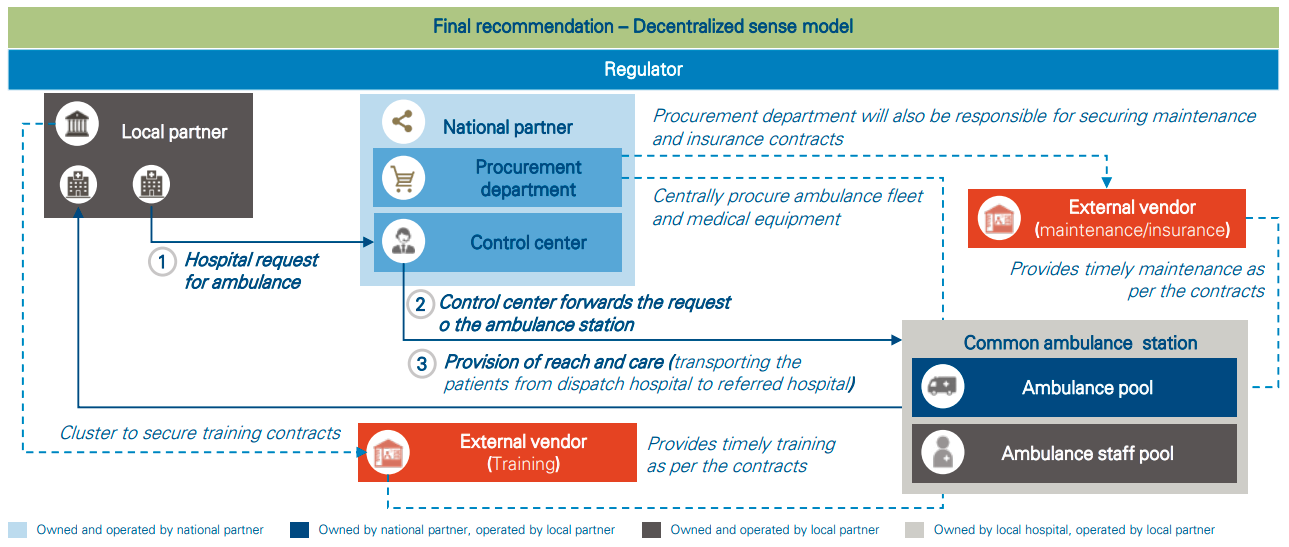
3. Assessing the developed options
Arthur D. Little used learning from benchmarked countries to recommend innovative solutions and applied the Triple-A framework, keeping in mind strategic alignment to recommend the optimal operating model.
DOWNLOAD THE FULL REPORT
11 min read • Healthcare & Life Sciences, Operations management
Ambulance services – Optimizing operations
Rethinking emergency services for efficiency

DATE

Executive Summary
The global ambulance service market is projected to exhibit steep growth, which will be linked primarily to an aging population, favorable payment policies, and an increase in road accidents. Ambulance service providers need to come up with novel methods to address this rise in demand.
In this paper, Arthur D. Little and Access Health propose a framework that enables concerned stakeholders to identify root causes of inefficiency and, consequently, develop operating models supported by innovative approaches and technologies.
Ambulance services across the globe can be classified into six categories based on criticality, urgency, source and destination, and stage of care. While developing an operating model for ambulance services, it is critical to set the scope of the services because different types should be measured with different sets of KPIs.
Understanding the value chain and the associated processes in each step is vital to building efficient operating models. Arthur D. Little, in partnership with Access Health, has developed the AMCA1 framework, which helps with critical analysis of the value chain. Deep and thorough understanding of all processes helps to customize the overall operating model to the requirements of different ambulance service categories.
All ambulance services can be mapped into two broad categories of assets: (i) control center and (ii) fleet and equipment; as well as four broad categories of related activities: (i) own, (ii) develop/ maintain, (iii) operate, and (iv) regulate. Arthur D. Little has developed its proprietary “Triple A” (Ambulance Asset and Activity) framework, which enables development of a strategically aligned and efficient operating model.
Building the best operating model for ambulance services based solely on efficiency carries the risk of ignoring factors such as the socio-economic construct, technological maturity of the ecosystem, institutional arrangements between different stakeholders, and involvement of private players.
Lastly, the recipe for a successful operating model is incomplete without innovative solutions. Arthur D. Little recommends developing solutions around the three key levers of ambulance operations: service delivery and asset development, governance and organization, and human capital development.
1
Categorize ambulance services
The global ambulance services market is projected to grow at a CAGR of 9.1 percent and reach approximately USD 50 billion by 20252 . This growth will be driven by three key factors: (i) aging population, (ii) favorable payment policies, and (iii) an increase in road accidents. Extensive growth such as the above can put excessive strain on existing resources, even to maintain the current performance. In order to improve performance levels and meet the increasing demand, ambulance service providers will have to deliver services with higher efficiency and sustainability, as well as improved customer experience.
Ambulance services across the globe can be classified into six categories:
- Pre-hospitalization transfer – emergency (PHT-E)
- Pre-hospitalization transfer – non-emergency (PHT-NE)
- Inter-facility transfer – critical (IFT-C)
- Inter-facility transfer – non-critical (IFT-NC)
- Post-treatment transfer (PTT)
- Large-scale gatherings or community events (Events)
These categories are based on:
- Criticality – refers to the patient’s condition and determines
- Urgency – refers to the time limit within which care should ideally be provisioned.
- Source and destination – refers to the location type from which the patient is picked up and handed over.
- Stage of treatment – refers to three different patient-care pathways. These are whether the patient has yet to be hospitalized for treatment, needs to be transported between facilities during the treatment, or must be transported back home post-treatment.
While designing the operating model, it is important to consider which category of service(s) is being planned for. If a provider is responsible for the full spectrum of services, it is imperative that the provider treats different categories as distinct business units with separate resources, while leveraging synergies between them.
Categorization is also useful from a performance management perspective. For example:
- PHT-E and NE should focus on patient outcomes, which might not be of similar significance for PTT and IFT-NC.
- IFT-C and PHT-E should focus on care provided during the ambulance journey, which might not be of similar significance for IFT-NC.
- PHT-E should focus on time to respond, which might not be of similar significance for PHT-NE and PTT.
2
Study the value chain and customize
Arthur D. Little has developed its proprietary framework, AMCA (refer to Figure 3), which enables providers to critically analyze the value chain for different types of ambulance services.
Accept – Receiving, accepting and prioritizing requests for ambulance services, and then assigning and dispatching the optimal vehicle and personnel to service each request.
Move – The process of reaching the patient’s location and transporting the patient to the appropriate healthcare facility.
Care – The process of providing care on the way to the healthcare facility, stabilizing the patient, and performing clinical handover at the healthcare facility.
Ask – Collecting feedback on ambulance services and storing the feedback data in a structured and usable format.
Each step along the value chain must be carefully customized for the category requirements. For example:
- Investing in expensive medical equipment for Care in IFT-C and PHT-E will help save lives, but similar investments in IFTNC or PTT would not be able to generate significant value.
- The same feedback questionnaire for Ask in PHT-E and IFT-NC will lead to longer questionnaires to ensure comprehensiveness, which will result in a collection of unnecessary and irrelevant data, as well as missing out on valuable insight.
Issues can be identified by deconstructing the ambulance services value chain into AMCA steps, which can be further broken down into specific process steps and KPIs. These issues can then be dealt with to maintain continuous improvement of services. For example, GVK Emergency Management and Research Institute in India has successfully ensured improvement of ambulance services for PHT-E in participating regions by clearly allocating different functions to different steps in the value chain. GVK EMRI’s impact, in the states where it operates, has improved KPIs in line with international benchmarks. For example, GVK EMRI operators can respond to 97 percent of requests on time and dispatch ambulances within an average of 90–120 seconds for emergencies
3
Enable each process with assets and activities
After establishing the process steps required to deliver one or more types of ambulance services, the next step is to identify the stakeholders involved in the ambulance services ecosystem, their respective responsibilities, and the specific contracts and interactions between them.
All types of ambulance services across the globe can be mapped into two broad categories of assets: (i) control center and (ii) fleet and equipment; as well as four wide categories of related activities: (i) own, (ii) develop/maintain, (iii) operate, and (iv) regulate. Arthur D. Little’s proprietary Triple A (Ambulance Asset and Activity) framework enables development of a strategically aligned and efficient operating model. The framework is based on the premise that each process can be mapped to one or more assets and activities for efficient delivery of services
There are four activities associated with each asset type:
Control center
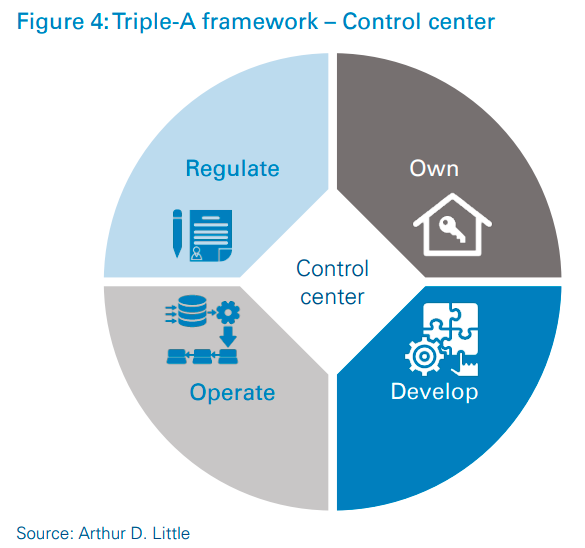
Own – Purchasing the fixed assets (except technology application) required for control center operations.
Develop – Working with a technology vendor to develop the technology solutions for control center operations.
Operate – Executing day-to-day control center operations, including hiring and training of the human resources required for them.
Regulate – Identifying performance KPIs and setting targets to ensure quality and efficiency of service. Ensuring robust performance measurement through audit and supervision.
Fleet and equipment
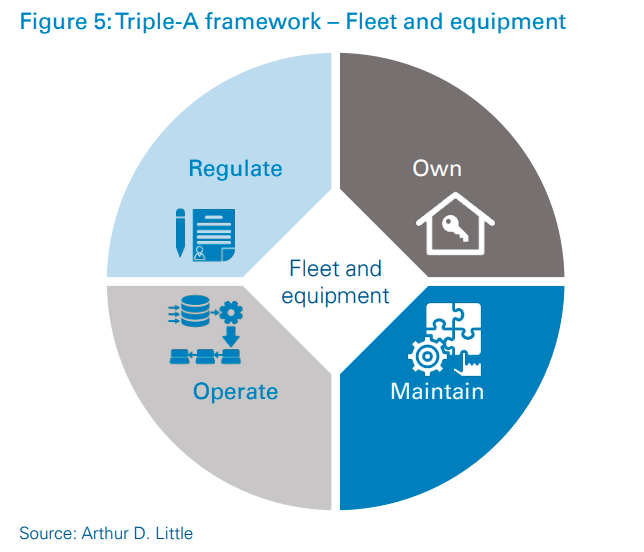
Own – Purchasing the fixed assets (vehicles and medical equipment) required for provision of ambulance move-and-care operations.
Maintain – Maintaining the ambulance fleet and medical equipment used for move-and-care operations.
Operate – Executing day-to-day move-and-care operations, including hiring and training the human resources required for them.
Regulate – Identifying performance KPIs and setting benchmarks to ensure quality and efficiency of service. Ensuring robust performance measurement through inspections.
The Triple-A framework can be used to develop strategic options for an operating model based on the divisions of activities within various stakeholder groups. The number and types of stakeholders identified can also vary between strategic options. Arthur D. Little has identified several parameters based on which each strategic option can be evaluated.
Investment required – The parameter for the efficiency of a model in terms of the investment required to set up and run operations.
Cost efficiency – The efficiency of the operations regarding the costs incurred when provisioning services.
Data-driven decision-making – The ease with which data can be collected and analyzed to enable continuous improvement.
Ease of implementation – The effort required for, and the feasibility of, implementing the option’s operating model.
Consistency of service – The degree of service standardization and consistency across regions.
Quality of service – The quality of service (call and care management) that the option’s operating model will be able to deliver
4
Consider the context
Efficiency might not be the most important factor in developing successful operating models. The right operating model must also consider other aspects, such the socio-economic construct, technological maturity, institutional arrangements between stakeholders, and involvement of private players and the community.
For example, a key factor to consider is the institutional arrangement between the national health ministry and the regional health administrations that are responsible for ambulance services. The operating model can be significantly different if the ministry is directly responsible for provision of ambulance services. As demonstrated above, it is important to identify the different institutional arrangements that provide and regulate ambulance services. It is also useful to consider which stakeholder is responsible for financing the operations and which is the payer for the services.
The governance model applied by the National Health Service (NHS) in England, where ambulance services are provisioned through autonomous regional NHS ambulance trusts, ensures effective governance of trusts without direct control. A national body within the NHS, NHS Improvement, benchmarks different trusts against each other, thereby creating a healthy competitive environment in which to learn and improve. As shown in the figure, NHS Improvement uses the Single Oversight Framework to assess trusts’ performance and support needs.
It is also imperative to set the context regarding the intended scale of services. For example, one needs to consider whether the model is being optimized for an ambulance operator with 20 ambulances, a hospital group with 100 ambulances, or a health ministry that provides ambulance services throughout a region or entire country.
Strategic alignment with the “big picture” of the healthcare system is a great example of how focusing solely on operational efficiency can risk long-term aspirations. For example, a healthcare system, which is centralized and wherein the onus of provisioning all types of services lies with the national health ministry, is trying to move towards a system of accountable care organizations (ACOs) based on regions. Assuming that a centralized ambulance service operating model is the most efficient, it will still be in the best interest of the country to choose a sub-optimal model in which a higher share of the responsibility lies with regional health administrations. Otherwise, the country risks hampering its progress towards an ACO model.
As exploring synergies is an immensely useful tool for optimization, it becomes important to identify providers and services with whom ambulance operators can work. For example, GVK Emergency Management and Research Institute in India, which drastically improved ambulance services in India, came up with a system of integrating operations with the police and fire departments to address life-threatening delays to emergency response services. According to GVK EMRI estimates, 18 percent of all emergency calls in India require police intervention. Hence, GVK EMRI ensured that three to six police personnel were stationed at emergency response centers. The move eliminated the need to wait for an emergency call to the police response number, as the personnel could be alerted based on a call to the ambulance number. GVK EMRI also integrated its technology with that of the police to enable the two departments to share valuable information in a seamless and efficient manner.
5
Success is driven by innovation
For an operating model to be optimal, development needs to be supported with innovation. Once each asset and activity is identified, relationships between them can be improved by innovating in the following areas:
- Service delivery and asset development
- Governance and organization
- Human-capital development
Based on an extensive benchmarking study of the most developed ambulance services across the globe, Arthur D. Little identified the following best practices across various areas to create a high-value-generating ambulance ecosystem:
Service delivery and asset development
Leverage technology
- Outsource technology to a technology vendor.
- Enable optimal geo-spatial positioning through technology.
- Use data analytics to identify issues and continuously improve.
Centralize operations
- Centralize services across relevant processes in the value chain for sizable cost reductions.
Improve asset quality
- Secure maintenance contracts with service providers/OEMs to ensure higher quality of fleet and medical equipment.
Governance and organization
Enforce guidelines
- Set comprehensive guidelines and regulations and ensure strict adherence.
- Ensure adherence to well-defined protocols at all levels for smooth and efficient service.
Measure and benchmark performance
- Conduct robust performance measurement, set targets, and link incentives to performance.
- Benchmark providers against each other to help them identify issues.
Structure organization by function
- Organize internal teams by different functions (such as human resources, finance, operations and technology) to achieve a lean and efficient organization structure.
Human capital development
Focus on career development
- Provide a clear career path for paramedical staff to assure them of long-term, sustainable careers and reduce turnover.
- Offer rotation of paramedical staff across units (regions, departments, etc.) to expose the workforce to valuable learning.
Improve access to formal education
- Ensure training of a sufficient number of paramedics by setting up educational institutes from scratch or leveraging existing institutes.>
Mandate continuing professional development
- Define minimum professional standards, conduct audits, and enable the system to upskill its talent
Arthur D. Little’s approach was designed to develop innovative and practical solutions based on careful assessment of the requirements, issues, and capabilities of the ambulance services in question. The assessment is followed by a rigorous benchmarking exercise that enables identification of best practices. We then help our clients develop operating models that take the context into consideration. As a last step, we provide tangible recommendations across the three key areas:
- Service delivery and asset development
- Governance and organization
- Human-capital development
We can support our clients from design to implementation of their ambulance services, depending on their internal requirements.
Case study
1. Categorizing services
The client organization was a GCC health ministry that acted as the regulator and national provider (focused on inter-facility ambulance services-referral transport).
2.Identifying key issues along the value chain
Arthur D. Little segmented the value chain as per the AMCA framework and identified key issues. The health ministry’s decentralized system suffered from problems such as low utilization of assets, shortage of trained paramedics, and low technology adoption.
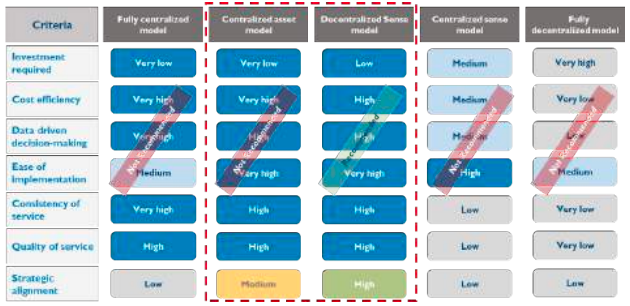
3. Assessing the developed options
Arthur D. Little used learning from benchmarked countries to recommend innovative solutions and applied the Triple-A framework, keeping in mind strategic alignment to recommend the optimal operating model.
DOWNLOAD THE FULL REPORT
