
DOWNLOAD
DATE
Contact
The healthcare sector is on the frontline of climate change, but while battling the effects of global warming on population health, it is also contributing to environmental damage. Without robust plans and decisive actions, the sector’s global emissions will triple in coming years and stretch health systems to a breaking point. This Viewpoint explores the pathway healthcare organizations can take to embed sustainability into their agendas, the benefits of doing so, and the challenges they need to overcome along the way.
There are fundamental, if not existential, threats that climate change, pollution, and resource depletion pose to human life. The impact of environmental damage on population health is evident in the world’s 7 million premature deaths a year due to air pollution and 600 million cases of foodborne illnesses.
Globally, pollution causes 27% of deaths from cardiovascular disease and 18% of cancer-related deaths, according to research from M.L. Brusseau et al. The impact of the healthcare sector on the environment has, however, been largely overlooked. Despite accounting for 10% of the world’s GDP, or US $7.2 trillion annually, the sector’s carbon footprint at 4.4% of global net emissions makes it the fifth-largest emitter of greenhouse gases (GHGs) in the world. Unless the healthcare sector takes action, its global emissions are expected to triple by 2050, reaching 6 gigatons a year.
While the concept of sustainability in healthcare has been around since the early 2000s, it has only recently come into the sharp focus of healthcare providers and regulatory authorities through its intersection with other priorities, such as the rising demand for health services, spiraling healthcare costs, quality of health outcomes, and patient satisfaction.
For these sector participants and their stakeholders, adopting environmentally friendly practices is not just a moral obligation, it is a strategic necessity with sizeable financial, reputational, and population health implications.
Sustainable healthcare is, according to the World Health Organization (WHO), “a system that improves, maintains, or restores health, while minimizing negative impacts on the environment and leveraging opportunities to restore and improve it, to the benefit of the health and well-being of current and future generations.” Many healthcare organizations are implementing sustainable healthcare practices to reduce their carbon footprint, make more sustainable use of their resources, and deliver results on the triple-bottom line of people, profits, and the planet.
THE SUSTAINABILITY IMPERATIVE IN THE HEALTHCARE SECTOR
In the words of WHO, “Places of healing should be leading the way, not contributing to the burden of disease.” Unfortunately, the healthcare sector’s environmental impact is profound due to its energy-intensive operations, waste generation, and extensive use of environmentally harmful materials, making it a significant contributor to GHGs at a national level (see Figure 1).
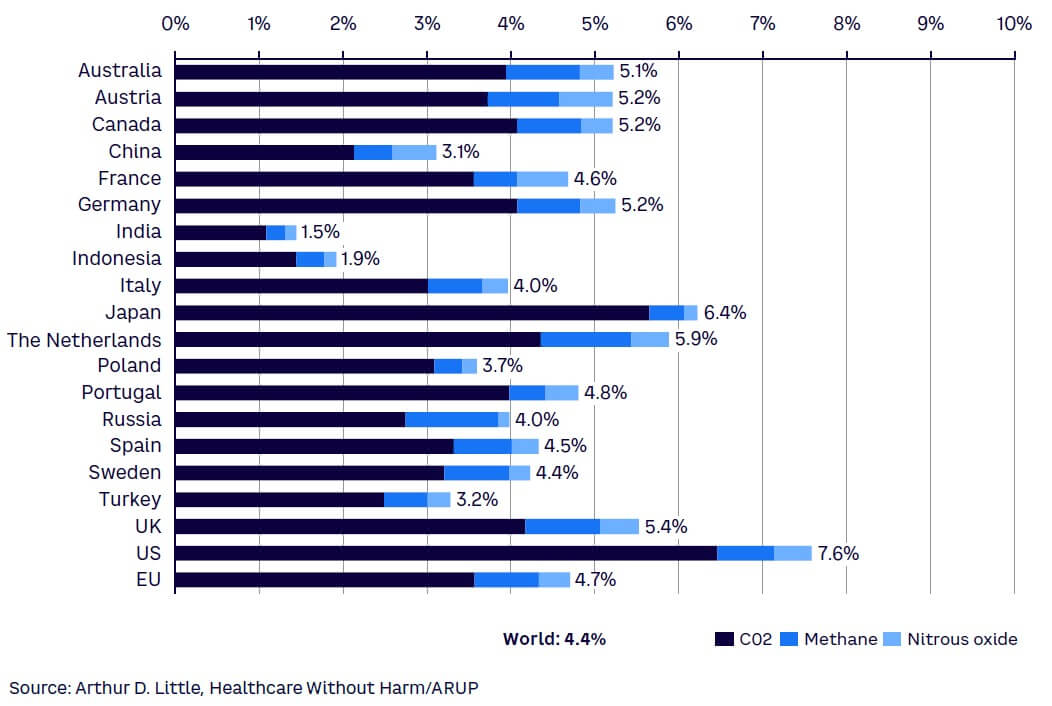
It is interesting to note that while China is the world’s highest GHG emitter in absolute terms, the US exceeds it in terms of its healthcare-related emissions. Although Middle Eastern countries are not shown in Figure 1, significant sustainability efforts are underway. Saudi Arabia for example, with carbon dioxide equivalent (CO2e) emissions estimated at 810 million tons per annum (MTPA) in 2022, aims to reduce its carbon emissions by 278 MTPA by 2030 and be net zero by 2060, as part of its Saudi Green Initiative (SGI). The health sector’s footprint will most likely be impacted by the Kingdom’s transition to renewable energy sources, commitment to a circular carbon economy in line with the Paris Agreement, and $200 billion investment to grow the green economy.
Healthcare facilities are the cornerstone of most health systems and where the sector’s environmental impact can most easily be observed. Hospitals, for instance, operate 24/7 and typically consume between 200-400 kWh (equivalent to 80-160 kg of CO2 in emissions) per bed, per year on energy for lighting, heating, ventilation, and medical equipment. The healthcare sector also generates substantial waste from single-use and disposable materials. Research shows that operating rooms, while occupying a relatively small physical area in a hospital, produce 20%-33% of a facility’s total waste.
Other studies estimate that 15% of hospital waste is hazardous and can be infectious, toxic, or radioactive, with hospitals in high-income countries producing up to 11 kg of hazardous waste per bed, per day, much of which is not biodegradable.
From a specialty perspective, orthopedics, oncology, cardiology, and neurology departments have the highest carbon footprint because of their extensive use of energy-intensive equipment (e.g., operating rooms, intensive care units, and diagnostic imaging), single-use materials, and gases. In nephrology, dialysis also contributes significantly due to high water and energy consumption. In the hospital-support functions, estates, IT, and catering stand out as the chief contributors.
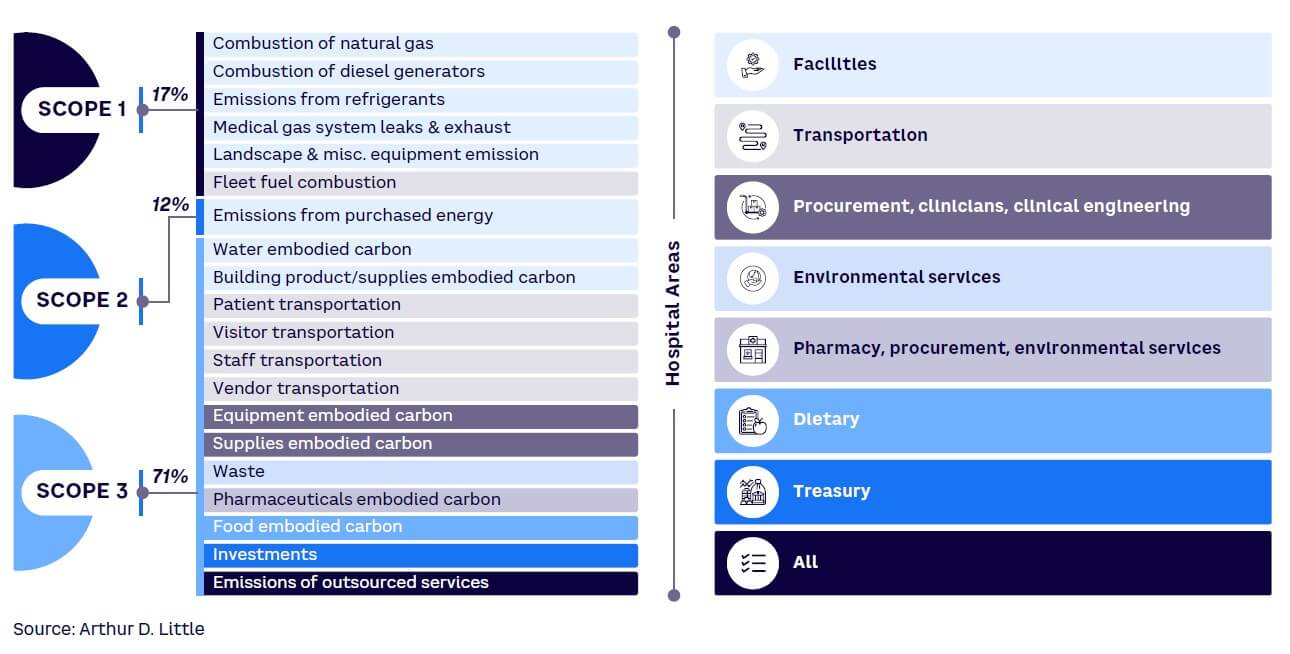
Figure 2 shows the contribution of different hospital areas to GHG emissions, split across Scope 1 (direct), Scope 2 (indirect via energy usage), and Scope 3 (all other indirect sources, including the supply chain). The scale of the problem is particularly dire beyond the walls of a hospital, with the healthcare supply chain responsible for over 70% of emissions, primarily from fossil fuel consumption in the production, transport, and disposal of drugs, devices, and supplies. A comprehensive approach that covers the entire value chain is therefore essential.
A LAYERED APPROACH CAN MAKE A DIFFERENCE
Arthur D. Little (ADL) encourages a structured approach to integrating sustainability within healthcare that focuses on three connected layers (see Figure 3).
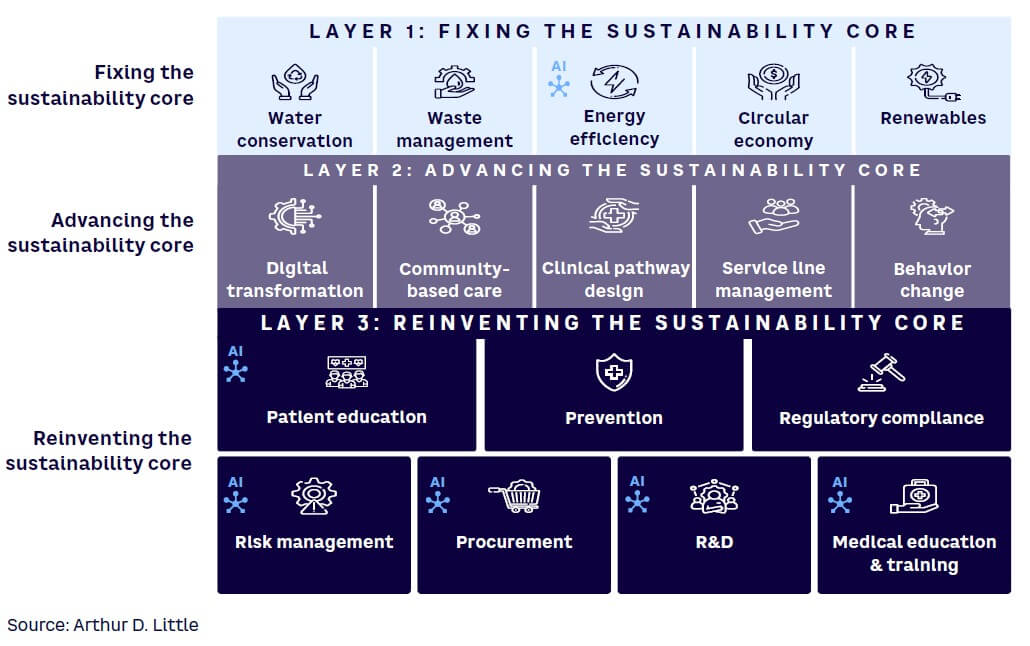
By addressing environmental, economic, and operational practices at all levels, from core principles to societal integration, we use a model that ensures healthcare institutions can systematically work toward their sustainability goals and realize long-term benefits at a facility, system, and population level.
Layer 1: Fixing the sustainability core
Our model starts by addressing fundamental practices, such as water conservation, waste management, energy efficiency, circular economy principles, and investment in renewable energy. Waste-to-energy systems that convert medical waste into usable energy, for example, offer a dual benefit of waste reduction and energy generation and have been successfully implemented by several European hospitals. These basic activities reduce the environmental footprint of healthcare operations and lay the foundation for sustainable progress, starting with Scope 1 and Scope 2 emissions.
Layer 2: Advancing the sustainability core
The next layer focuses on broader operational areas, including digital transformation, community-based care, clinical pathway redesign, behavioral change, as well as service line management that further impacts Scope 1 and Scope 2. Digital enablement in the form of telemedicine, for instance, has been increasingly adopted, particularly during the COVID-19 pandemic. Virtual consultations reduce the need for physical visits, decreasing carbon emissions associated with transportation but also lowering the demand for physical infrastructure, such as clinic space. The adoption of AI-driven diagnostic tools can help minimize unnecessary tests and procedures thereby reducing the consumption of resources and the need for patient visits. More robust demand prediction can also minimize wastage from unused short shelf-life drugs and supplies.
Redesigning the model of care to focus on well-being and healthy living, as well as care in alternative settings, can reduce resource consumption and the number of hospital visits and enhance patient experience and convenience. Linked to this, standardized clinical pathways build upon other sustainability measures by streamlining care processes and reducing unnecessary interventions, leading to more efficient resource use and minimized waste. They can enhance resource utilization through optimized staffing and scheduling, optimize patient flow, and reduce the need for avoidable medication, patient tests and travel, lowering the environmental impact of healthcare.
Layer 3: Reinventing the sustainability core
The third layer targets more complex challenges that require stakeholder alignment, such as patient education, procurement, regulatory compliance, and risk management. Additionally, it focuses on long-term enablers like prevention, medical education, and R&D to ensure sustainability becomes deeply integrated into healthcare delivery.
From a risk management perspective, AI-enabled wearable devices, for example, can monitor patient health in real time, predicting potential health issues before they escalate. In post-discharge scenarios, they can help prevent avoidable readmissions and lower the resources consumed through emergency visits and re-hospitalization.
With Scope 3 emissions accounting for around 70% of the sector’s GHGs, procurement is key to greening the healthcare supply chain. As discussed in the ADL Viewpoint, “ From Source to Sustainability: Decarbonizing the Supply Chain,” procurement teams must collaborate with suppliers to improve transparency and reduce emissions. Balancing sustainability with cost, quality, and performance requires thoughtful compromises. Healthcare organizations can adopt eco-friendly procurement strategies, focusing on reducing single-use plastics, sourcing sustainably, and ensuring supplier adherence to environmental standards.
R&D can also leverage AI to minimize resource consumption and environmental waste in the clinical trials and drug discovery process. The ADL Viewpoint “Accelerating Cures” presents how AI can swiftly analyze real-world data for patient matching, use social media to determine patient clusters, prescreen individuals, and apply graph networks to identify pre-diagnosis patients. This can lead to a more streamlined process that optimizes innovation with sustainability goals.
Increasing physicians’ awareness of healthcare’s environmental impact and integrating best practices into medical education and training is essential for promoting sustainability. Introducing AI tools, for example, can help clinicians make more accurate diagnoses and choose optimal treatments, resulting in faster recoveries and reducing the need for extensive procedures, ultimately leading to lower resource consumption.
REALIZING BENEFITS
Multiple benefits can be realized by integrating environmental, economic, and operational practices that enhance the efficiency of healthcare systems while ensuring positive outcomes for patients, staff, and the environment. These include:
- Economic savings. Sustainability helps realize cost savings over the long term by optimizing resource efficiency in areas such as energy, water, and waste management. These can reduce operational costs, while regulations can incentivize healthcare facilities to adopt innovative technologies and environmentally responsible practices. By embracing these changes, healthcare institutions can reduce waste, transition to energy-efficient technologies, and ultimately lower their operational expenses.
- Environmental benefits. Reduction of GHG emissions and pollution not only minimizes the sector’s ecological footprint, it also contributes to improved public health outcomes by fostering cleaner and safer healthcare environments.
- Patient care. Sustainability is linked to improved quality of care, creating safer environments for both patients and healthcare staff by reducing exposure to harmful substances. Sustainable practices promote the use of safer materials, and their alignment with preventive care strategies fosters healthier lifestyles that can reduce long-term healthcare demand. These efforts can also improve patient experience and convenience, as well giving them more choice.
- Public image and reputation. The adoption of sustainability practices also enhances a healthcare institution’s public image and reputation as a responsible entity committed to environmental responsibility and social well-being. By integrating sustainability at every level, from infrastructure to daily care delivery, healthcare systems can safeguard their future while continuing to maintain high standards of care and operational efficiency.
- Regulatory compliance. The importance of sustainability in healthcare will increase as governments introduce stricter environmental regulations. Healthcare organizations that take proactive steps toward integrating sustainability into their operations, provide sustainability reporting, and ensure compliance to standards will be better positioned to meet requirements and avoid potential fines or penalties. In recent years, regulators have imposed fines on a number of hospitals for violating hazardous waste regulations, and in the case of one UK National Health Service (NHS) hospital, for exceeding its carbon emissions target.
OVERCOMING CHALLENGES
Despite the clear necessity for sustainable practices, healthcare organizations face considerable challenges, including:
- Cost and investment. There can be an immense financial burden associated with upgrading existing, often aged facilities with energy-efficient systems. Payback periods may be long, requiring a strong strategic focus supported by a robust business case. The dilemma between investing in care or investing in the environment, given short-term capital funding constraints, can sometimes be alleviated through public-private partnership/private sector partnership (PPP/PSP) contracts and partnerships, which can also give access to best-practice solutions.
- Data availability and quality. Gathering accurate and reliable data on an organization’s carbon footprint, and the Scope 3 emissions of suppliers, can be challenging due to data availability, consistency, and transparency issues.
- Organizational change. Changing working practices and cultural norms in a healthcare setting can be especially challenging and require a concerted effort to educate and align clinicians, staff, and patients on the benefits of sustainability. This can be achieved through training and education, communications, and incentives to encourage and support the adoption of sustainability measures.
- Regulatory compliance. Healthcare organizations must navigate a complex regulatory environment that includes stringent health and safety standards. Any changes to operations, such as the adoption of new waste management systems or energy-efficient technologies, must comply with these regulations, which can slow down the implementation process.
- Stakeholder engagement. Engaging suppliers and other stakeholders in emissions-reduction initiatives can be challenging due to varying levels of commitment, capabilities, and priorities.
- Supply chain complexity. Managing emissions across a complex value chain involving numerous suppliers and partners requires coordination, data sharing, and collaboration. Identifying and selecting suppliers with low-carbon footprints and sustainable practices may require extensive supplier evaluation processes and potential adjustments to supply chain policies and relationships.
A PRACTICAL PATHWAY
To embark on the journey to sustainability, healthcare organizations need to first understand their GHG profile (expressed in CO2e). Based on this, they can then develop targets and management plans that address their Scope 1, 2, and 3 GHG emissions. We recommend healthcare organizations take the following three steps:
- Analyze and plan. Begin by securing leadership support and commitment to emissions reduction. The case for change can be prepared by studying the organization’s existing emissions sources and trends and pinpointing priority areas for improvement. This information can then be used to establish targets aimed at reducing emissions and minimizing waste. Measurement mechanisms and KPIs should then be established so that progress and ROI can be routinely monitored and appraised. Finally, stakeholders should be engaged to foster collective support in reducing the organization’s footprint.
- Improve healthcare delivery and facilities (Scope 1 & 2). The next step is to develop an operational plan that defines specific initiatives and their implementation timelines. The various aspects mentioned in Layer 1 and Layer 2 of our model can be selectively adopted (e.g., redesigning the patient pathway and clinical model of care to promote early detection, treatment, and care in alternative settings). Organizations should also foster a culture of sustainability within the organization that empowers staff to actively participate in decarbonization efforts. Hospitals should educate staff on best practices and raise awareness through internal campaigns.
- Adapt the healthcare supply chain (Scope 3). The final step is to work with stakeholders in the broader health ecosystem who can contribute to the organization’s environmental goals. These can include patients and regulators, as well as medical colleges and suppliers, through measures identified in Layer 3 of our model. For example, by collaborating with suppliers, sustainability practices can be integrated at every stage of the supply chain, from sourcing raw materials to delivering products and managing waste. By embedding sustainability into procurement processes, healthcare organizations can significantly lower their GHG footprint and promote a more eco-friendly supply chain.
THE NEED FOR STAKEHOLDER COORDINATION
Of course, improving sustainability in the healthcare sector isn’t achievable from healthcare providers alone. It requires the coordinated efforts of all sector stakeholders, including regulators, payers, and suppliers, each playing a critical role.
Regulators
- Mandate standards that encourage existing facilities to modernize and upgrade and issue regulations to guide the development of new facilities.
- Introduce regulations for healthcare facilities to report their emissions targets and performance. These regulations should set clear, measurable goals and timelines, with regular audits and penalties for noncompliance.
- Support R&D in energy-efficient technologies and renewable energy sources. This can reduce the reliance of fossil fuels in providing energy for healthcare systems.
- Facilitate partnerships and PPP/PSP contracts and provide incentives like sustainability credits, grants, or tax breaks for hospitals meeting emission standards.
Payers
- Design pricing models that reward hospitals for implementing sustainable practices. Premiums can be reduced for hospitals that meet targets to encourage widespread adoption of carbon-reduction efforts.
- Support initiatives like sustainability credits or offering lower premiums for hospitals meeting emission standards. This can create a competitive advantage for “green” hospitals.
- Partner on projects or fund sustainable upgrades to help reduce overall healthcare costs. Payers should work with hospitals to develop joint initiatives that align sustainability objectives along with premium healthcare standards.
Suppliers
- Provide sustainable products to healthcare organizations that are manufactured with low-carbon processes, use sustainable materials, and minimize packaging waste. Suppliers can help end users reduce their supply chain emissions by providing green alternatives.
- Ensure transparency in supply chain emissions and provide data on the carbon impact of their products. Healthcare organizations should be able to make informed purchase choices according to information on how the materials were sourced, produced, and delivered.
- Partner with hospitals on joint sustainability initiatives such as developing eco-friendly products, reduce transportation emissions and disposal costs, and co-invest in capital projects. Joint efforts can lead to mutual benefits and drive innovation within the supply chain.
Conclusion
SUSTAINABLE HEALTHCARE: BETTER FOR BUSINESS, PEOPLE & THE PLANET
Sustainability in healthcare is a strategic imperative that can drive cost savings, enhance patient care, and improve an organization’s reputation with stakeholders. By investing in green technologies, optimizing supply chains, and adopting sustainable practices, healthcare organizations can significantly reduce their environmental impact while maintaining or even improving the quality of care they provide.
We encourage healthcare leaders to take immediate steps toward sustainability by conducting thorough assessments of their operations and committing to long-term sustainability goals. Now is the time to act, and the benefits are clear. By integrating sustainability into their core operations, healthcare organizations can contribute to a healthier planet and ensure their own long-term success in an increasingly competitive and environmentally conscious world.


