Following on the heels of other industries, the healthcare sector is undergoing a critical transformation to become data driven. As this revolution comes to the forefront, technology trends are emerging, but other interconnected factors related to both how data is gathered or analyzed and how stakeholders are involved can enable or hinder the change.
Everything is digital, but healthcare a little less so.
We are living in an era where every activity of our lives is going digital. So how does that impact the healthcare industry when, primarily, the success of any health organization requires the pursuit of three aims:
- Quality – guaranteeing the effectiveness of care and improving the experience of patients.
- Access – providing proactive care or facilitating entry into the healthcare system upon recognizing a need.
- Efficiency – improving healthcare processes and reducing per capita costs of healthcare while guaranteeing quality and access.
The digital transformation of healthcare is key to achieving these objectives, especially since this industry lags sectors such as media, financial services, and wholesale trade, which have gained clear advantages from global digitalization. For instance, in Italy, as reported by Gilead Sciences, when dealing with personal health, over 50% of the population prefers to see a doctor in person rather than remotely. Indeed, according to our analysis, people miss human contact when interacting with an artificial intelligence (AI) system. Moreover, healthcare facilities approve few digital initiatives, and a significant number of these facilities have not even introduced relevant new technologies in their strategic plans. In fact, healthcare facilities in 2019 invested half of their IT budget in software and hardware maintenance, while directing just 7% toward AI and big data projects, according to AGID, the Italian government’s digital agency.
From digital health to data-driven healthcare
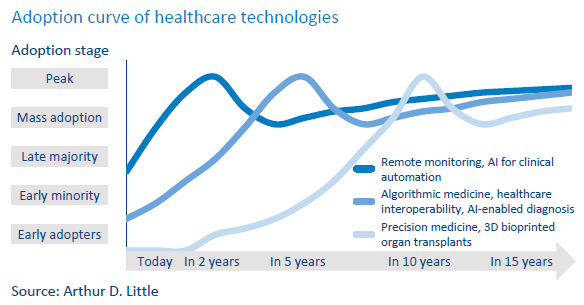
New definitions of eHealth and digital health are continuously emerging. The World Health Organization (WHO) defines eHealth as “the use of information and communication technologies for health,” while digital health is described more broadly as an umbrella term covering areas including eHealth, telehealth, and more. During the next decade, the healthcare industry will undergo a profound transformation as many important technologies, including AI, reach mainstream adoption. Clinical workflow will become more agile by virtue of AI and advanced analytics that automate decision-making processes. The emergence of these technologies requires a transformation from mere digital health to data-driven healthcare given the fundamental role of data in automated decision making (see figure below).
Big data, in particular, is the trigger to move the healthcare industry forward. Big data analysis aggregates information and makes possible the identification of patterns and trends. For the healthcare industry, big data can provide several important benefits, including:
- More accurate staffing – helps hospitals estimate future admission rates.
- Facilitation of chronic care – facilitates effective management of a population risk cohort by creating lean processes for continuous and standardized treatments.
- Lower rate of medication errors – can identify and flag any inconsistencies between a patient’s health conditions and drug prescriptions and alert health professionals and patients of any discrepancy
Drivers of data-driven healthcare
In the shift toward data-driven healthcare, focusing only on new technologies is not sufficient. Indeed, how data is gathered and how stakeholders’ interests are managed can enable or hinder the transformation. As illustrated in the figure below, we have identified eight drivers of data-driven healthcare, which can be positive or negative.

1. Technology trends
Today’s technology already enables clinicians and patients to engage more effectively together to improve health outcomes, and access to health technology is becoming a commodity. Indeed, the growing acceptance of wearable medical devices and the cloudification of the healthcare industry support the increasing use of electronic health records:
Wearables. Consumer wearables are on the rise for remote medical monitoring, with the use of medical-grade mobile devices to actively monitor patients’ conditions.
Cloudification. Cloud-based storage and applications allow better communication between care teams, leading to improvement of clinical outcomes and patient experience.
These ongoing trends provide an essential foundation for the next generation of innovations, including the use of AI and precision medicine, which involves the combination of big data analytics and machine learning (ML) algorithms.
2. Data quality and availability
New technological devices generate huge amounts of data that can be analyzed to provide real-time clinical or medical care. To extract value from big data, the major challenge is how to make it relevant, actionable, available, and interoperable:
- Relevance. First comes the identification of the data needed to derive insights that promote the attainment of organizational goals. To do so, it is important to start with a business question around which to center the data initiative.
- Actionability. Data should provide enough insights into the future so that it becomes clear to decision makers what actions they should take. To make data actionable, data collected must be clean, complete, accurate, and correctly formatted for use across systems.
- Availability. All data necessary for efficient analysis should be easily accessible to, and readable by, the scientific community. Incorrectly defined sharing restrictions can prevent skilled healthcare professionals from accessing pertinent patient information.
- Interoperability. To obtain a complete view of a patient, healthcare professionals need to regularly look through data from multiple sources. For thorough data analysis, health systems should be consolidated through the definition of a homogenous communication standard.
3. Data security
Given the massive amount of data and its value in the health sector, it is of great importance to ensure security. Data security in healthcare is complex with the aims of ensuring the secure exchange of patient information, protecting the integrity of medical applications, and controlling access to healthcare applications and systems holding personal data. Data security affects the entire healthcare ecosystem; therefore, technical measures alone cannot be a solution.
For an adequate level of data protection, it is vital to act at an organizational level, setting up a dedicated corporate figure/committee to
- monitor and assess regulatory compliance for data processing,
- define and update data management policies,
- provide training for those dealing with health data, and
- implement “secure by design” information systems. Moreover, transformation toward data-driven healthcare is not limited to how data is gathered and analyzed but also involves all stakeholders in the ecosystem, including government, patients, partners, and suppliers of healthcare providers.
4. Enabling ecosystem
To stimulate the development of data-driven healthcare, government must design a digital health strategy that pursues the following goals:
- Support the availability of healthcare technologies and their development by facilitating investment from both public and private industry players.
- Boost innovation by encouraging knowledge sharing through the creation of points of contact between stakeholders.
- Encourage the creation of an integrated healthcare system focused on the patient by providing easy and broad access to information.
- Promote cultural transformation and raise awareness of digital health among healthcare workers and patients.
In addition, government must assign key importance to the right to protect personal data. This right, enshrined in numerous international norms and standards, provides that individuals may request that their personal data be collected and processed by third parties only in compliance with relevant legislation. In Europe, the processing of personal data is regulated by the General Data Protection Regulation (GDPR) and by the regulations of individual countries. For personal health data, GDPR aims to give the data subject the power to manage his or her own data, guaranteeing control over all information, including the provision of healthcare services revealing personal information.
5. Public-private partnerships
Public-private partnerships are established specifically to harness the potential of big data in healthcare and include partners working across the data chain. Collaboration between the public and private sectors to analyze biomedical data raises some specific ethical issues:
- Legislative framework. In areas of rapid change, such as data science, practice can quickly outstrip the regulatory framework. Stakeholder acceptance of a given data use should be clearly defined.
- Data ownership. Partnerships provide the chance to appropriate public data sets or extract value from accessing public data. This raises questions of ownership for both raw data and research outputs.
- Commercialization of research results. The public may be hostile to the use of health data for commercial gain.
To ease ethical tensions regarding public-private partnerships’ use of biomedical big data, it is important to articulate and share openly how the partnership will produce public benefit and how benefits will be distributed within the community.
6. Patient participation
People concerned about their own care are leading the rise of data-driven healthcare. However, individuals are not always willing to share their health data with companies or the government for various reasons:
- Personally identifiable information. People are reluctant to share sensitive information.
- Retention period of data and third-party access. The more institutions demonstrate their ability to process data, the less people are likely to share their data.
- Scope of use of data. If people do not understand the benefits of sharing data, they will not share it.
We see reluctance to share health data when looking at the uptake of contact-tracing apps developed to help reduce the spread of COVID-19. From June to October 2020, only 7 million people downloaded the Italian contact-tracing app Immuni. The app targeted every Italian who owns a smartphone, or almost 44 million people, but according to the research institute CENSIS, the market penetration index was around 16%, a result below expectations, according to the Italian Ministry of Health.
7. Change management in the healthcare industry
A key factor hindering the transformation of the healthcare industry is its resistance to change. Sources of this resistance arise within a change effort both when formulating the change initiative and when implementing it:
- Atomistic view. Individual units fail to recognize that the overall quality of care for patients involves more than their individual effort.
- Embedded ideas. There is a tendency to continue with current thoughts and routines despite changing situations.
- Organizational culture. Many healthcare professionals believe they can drive change, but hierarchical structures hamper their ability
Resisting change is common within healthcare organizations, given the implementation of generally tight and timeconsuming procedures. Any type of change effort impacting patient treatment and care needs to go through many levels of management approval before official implementation.
8. Skills development
If the healthcare industry still has a long way to go in terms of the percentage of available data that is actually put to use, this is partly due to lack of data analysis skills. Insufficient data analytics talent has been a perennial pain point for the healthcare industry, which has struggled to develop the competences required to extract valuable insight from big data.
While many organizations are starting to bridge the divide between data creation and data analytics, employees with data analytics competencies and extensive training in the intricacies of healthcare data are in high demand. Data analysts, data managers, and data stewards are needed to manage the gathering and analysis of data, while developers skilled in Agile methodologies (e.g., Scrum) are needed in software development.
Case study – Lombardy Region and the Digital Information Hub
With the objective of helping the transition toward data driven healthcare, Aria, a public limited company supporting innovation in the Lombardy region of Italy, launched the Digital Information Hub (DIH) to connect different stakeholders in the regional ecosystem. DIH focuses on providing public institutions with meaningful healthcare data to carry out crucial research. Initially, it granted access only to aggregated patient health data gathered by local healthcare operators. Arthur D. Little was involved in the design of the service concept, the definition of the service strategy, and early experimentation with the new service model.
Given the need to share sensitive data, it was necessary to deal with many issues described in this Viewpoint. Local authorities first defined a dedicated regulation to guarantee data anonymity and protection from data breaches, which has been enforced operatively using specific technological solutions. Next came the decision that access to the DIH platform should be granted only to public institutions willing to share the benefits of the research with the community. Currently, through the development of several data science tools, DIH also supports institutions during data analysis. Innovative applications of emerging technologies like ML that allow the analysis of larger data sets are being examined and will be implemented in future evolutions of the platform.
Conclusion
The healthcare industry faces change in the next years to transform patient care. In this early stage of this revolution, trends such as growing acceptance of wearable healthcare devices, cloudification, and the incorporation of AI into healthcare are coming into play. These new technologies generate a massive quantity of data that must be processed and secured to create value.
Various stakeholders are driving the transformation of the healthcare industry. Government can promote the implementation of integrated systems and knowledge sharing, while private institutions may supply specific analytics skills. However, individuals are, in some cases, reluctant to share data if they are unable to benefit from it. Finally, the culture within healthcare organizations and the lack of appropriate analytics skills may impede change.
Arthur D. Little supports the healthcare industry in the design and implementation of a data-driven business model that values information assets to achieve the triple aim of quality, efficiency, and access while considering all the drivers, both positive and negative, discussed in this Viewpoint.